The female reproductive system is a marvel of biological sophistication, making it a subject of intrigue for both scientists and the general populace. It is within this system that one critical event occurs monthly: ovulation, the release of a mature oocyte from the ovary. This event is fundamental to reproduction, yet many individuals possess a limited understanding of the specific cell type that is actually ovulated. Understanding this aspect can deepen one’s appreciation of reproductive biology and the intricate processes governing fertility.
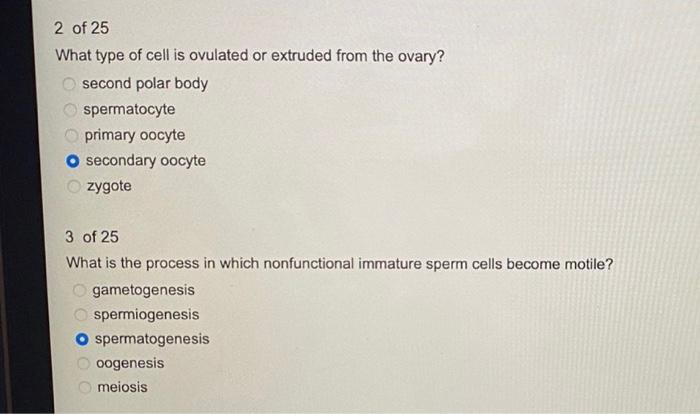
At the core of ovulation lies the oocyte, which is the haploid cell central to egg formation. However, it is essential to recognize that what is ovulated is not merely the oocyte itself, but rather a more complex structure called the secondary oocyte. This distinction is crucial for a comprehensive understanding of reproductive biology.
To delve deeper, we must first examine the development of ovarian follicles, which are integral to oocyte maturation. Within each ovary, oocytes are housed in structures known as follicles, characterized by a layered architecture comprising granulosa cells and theca cells. The developmental trajectory of the follicle is marked by several stages: primordial, primary, secondary, and tertiary follicles. Each stage serves a distinct purpose in nurturing and preparing the oocyte for potential fertilization.
During the early part of the menstrual cycle, a cohort of follicles is stimulated by follicle-stimulating hormone (FSH). Interestingly, although multiple follicles may begin to mature, typically only one achieves full maturity and is poised for ovulation. The selected follicle is termed the Graafian follicle, which engenders a dramatic enlargement while secreting increasing quantities of estrogen.
As estrogen levels rise, they exert a feedback effect on the hypothalamus and pituitary gland, culminating in a surge of luteinizing hormone (LH). It is this hormonal cascade that triggers the ultimate maturation and release of the secondary oocyte. The oocyte, now enveloped by a layer of granulosa cells, is expelled from the ovary during ovulation, seamlessly entering the fallopian tube, where it awaits fertilization.
At this juncture, it is imperative to elucidate the characteristics of the secondary oocyte. This cell is distinguished from the primary oocyte by its completion of meiosis I, resulting in the formation of two haploid cells: the secondary oocyte and a smaller polar body that usually degenerates. The secondary oocyte is arrested in metaphase of meiosis II, remaining in this state until fertilization occurs. This pause in development adds a fascinating layer of complexity to the ovulatory process.
The arrest of the secondary oocyte at metaphase II can be interpreted as an evolutionary strategy to maximize reproductive success. By delaying the completion of meiosis until the moment of fertilization, the female reproductive system optimizes the chances of successful fertilization, particularly in the context of sperm availability and viability.
The actual process of ovulation is an equally intricate phenomenon. It does not merely entail the rupture of the follicle but also the coordinated activity of several hormones and enzymes. The enzymatic activity, particularly of proteolytic enzymes, plays a pivotal role in weakening the follicular wall, facilitating the release of the oocyte. Additionally, the cumulus oophorus, a cluster of granulosa cells surrounding the oocyte, plays an essential role in guiding the released oocyte towards the fimbriae of the fallopian tube.
Furthermore, the environment in which ovulation occurs is meticulously orchestrated. The ovary undergoes a series of physiological changes, including increased blood flow and a rise in local temperature, to support the ovulation process. This environment is conducive not only to the release of the oocyte but also to the immediate interactions with sperm, should fertilization take place.
Despite the apparent simplicity of the ovulation process, numerous factors can influence it. Hormonal imbalances, irregular menstrual cycles, and various physiological conditions can disrupt normal ovulation, leading to implications for fertility. PCOS, or polycystic ovary syndrome, is one such condition that showcases the complex interplay of hormones and their impact on oocyte maturation and release. Understanding these dynamics is crucial for addressing reproductive health issues.
In conclusion, while the term “ovulated cell” might lead to the simplistic identification of the oocyte, it is essential to acknowledge that what is released is the secondary oocyte, a cell intricately designed for the uncertainties of reproduction. The secondary oocyte, its unique characteristics, and the elaborate process that governs its release are paramount in the broader context of female reproductive biology. As we cultivate a deeper knowledge of these mechanisms, we not only enhance our scientific literacy but also foster a profound respect for the complexities of life itself.
