When considering antibiotics, have you ever pondered the underlying question: can these seemingly benign medications affect your blood pressure? The answer is not only intriguing but potentially essential for your health management. As we explore this critical subject, we will delve into the myriad of antibiotics and their assorted side effects — particularly their potential interplay with blood pressure levels. Knowing the ramifications can pose a considerable challenge, yet it is a necessary endeavor for anyone prescribed antibiotics.
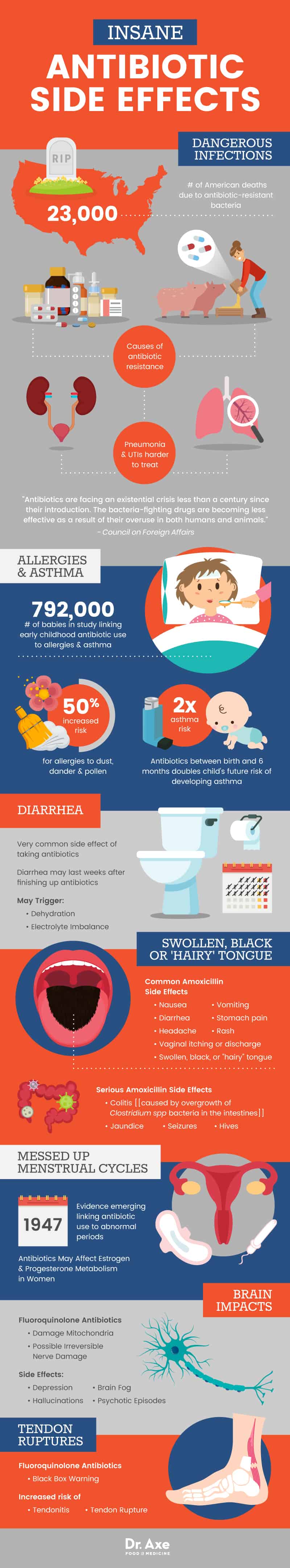
First and foremost, understanding the mechanism of antibiotics is imperative. Antibiotics are designed to combat bacterial infections by either killing bacteria or inhibiting their growth. Despite their lifesaving attributes, they do have collateral side effects, including those that can indirectly or directly influence blood pressure. Such side effects are often multifaceted and can manifest differently among individuals, particularly in those with pre-existing hypertension or other cardiovascular conditions.
To delve deeper, we must examine various classes of antibiotics and their side effects pertaining to blood pressure. Each category serves as a unique archetype of antibiotic intervention, but they do share a similar potential for adverse reactions.
1. Penicillins: This widely used group includes amoxicillin and penicillin G. While primarily recognized for their efficacy against bacterial infections, they have been associated with moderate side effects, such as allergic reactions that occasionally precipitate hypotension (low blood pressure). In rare cases, the reaction can escalate into anaphylactic shock, presenting an emergency that creates a sharp decline in blood pressure levels.
2. Macrolides: This group, which encompasses medications like azithromycin and clarithromycin, inhibits bacterial protein synthesis. While their principal side effects involve gastrointestinal disturbances, a lesser-known consequence may include cardiovascular events. Azithromycin, for example, has been associated with QT prolongation, a heart rhythm condition that may ultimately lead to hypotension in susceptible patients.
3. Tetracyclines: Doxycycline and tetracycline are well-known examples in this class. Their primary side effects are gastrointestinal, but they can also induce esophageal irritation. If this irritation leads to severe discomfort or pain, it could cause a stress response that indirectly might elevate blood pressure. Although significant hypertension is less common, it’s essential to note any adverse reactions during the treatment process.
4. Fluoroquinolones: This class includes ciprofloxacin and levofloxacin, often prescribed for more severe infections. Notably, these antibiotics can cause central nervous system side effects, potentially leading to changes in mood and behavior that might inadvertently increase blood pressure due to stress or anxiety. Furthermore, there is some evidence suggesting that fluoroquinolones could affect glucose metabolism, which indirectly ties into cardiovascular health and blood pressure regulation.
5. Sulfonamides: Sulfamethoxazole is a popular example. This antibiotic can cause allergic reactions, which, although rare, might trigger hypotensive episodes. Additionally, if someone has a pre-existing condition like kidney disease, the use of sulfonamides may worsen renal function, thereby complicating blood pressure management.
6. Nitroimidazoles: Metronidazole is a staple in treating anaerobic infections and certain parasites. One key aspect often overlooked is the potential for cardiovascular side effects. Vertigo or dizziness experienced while on this medication could lead to orthostatic hypotension — a sudden drop in blood pressure when standing up — presenting a challenge for daily activity and stability.
Monitoring and Management: Given these risks, how can patients navigate the complex terrain of antibiotic therapy while safeguarding against potential blood pressure fluctuations? Here are some paramount strategies:
- Communicate With Your Healthcare Provider: Before starting any antibiotic regimen, informing your physician about any history of hypertension or cardiovascular issues is crucial. A comprehensive dialogue ensures that the chosen antibiotic does not exacerbate existing conditions.
- Regular Monitoring: Once on antibiotics, regular blood pressure monitoring can help detect any shifts early. This vigilance is particularly crucial for those whose blood pressure is already in flux.
- Be Aware of Symptoms: Understanding the signs of both hypotension and hypertension can equip you to respond effectively. Dizziness, fainting, or unusually high readings should prompt an immediate consultation.
- Alcohol and Caution: Combining certain antibiotics with alcohol can exacerbate side effects, including those affecting blood pressure. It is wise to limit or abstain from alcohol consumption during treatment.
Ultimately, the dialogue surrounding antibiotics and their side effects on blood pressure is more intricate than it may initially seem. While antibiotics save lives, the path to recovery can become convoluted if blood pressure variances are not anticipated and appropriately managed. Consider this a clarion call for patients to arm themselves with knowledge and engage proactively in their healthcare journey.
In conclusion, understanding how various antibiotics can influence blood pressure is not merely an academic exercise; it is a vital component of patient health awareness. While the medications may appear deceptively straightforward, their effects can ripple throughout the body, impacting more than just the targeted bacterial infections. Being informed is your best defense in mitigating risks and enhancing outcomes.
