The intricate tapestry of human development is woven with threads of maternal immunity, an enchanting process that beautifully illustrates the bond between a mother and her unborn child. Within this biological symphony, certain antibodies perform a poignant role, transcending barriers and bestowing protection in a journey from one life to another. This article delves into the fascinating world of antibodies, particularly focusing on the one that elegantly crosses the placenta—IgG—illuminating the profound implications for maternal and neonatal health.
When discussing antibodies, it is essential to recognize that they are not merely proteins; they are the vigilant sentinels of the immune system. The body produces various types to combat pathogens, each with distinct characteristics and functions. Among them, Immunoglobulin G (IgG) stands out as the versatile hero, adept at traversing the placental barrier, a feat akin to a skilled acrobat navigating a complex high-wire act.
The placenta, a remarkable organ, serves as a bridge between mother and fetus, facilitating nutrient exchange and waste removal. However, its role extends far beyond sustenance; it also defines the realm of immunological protection. Comprising a complex interface of cells, the placenta intricately regulates what passes through, selectively allowing certain immunological agents to reach the developing fetus. This selective permeability is where IgG orchestrates its essential function.
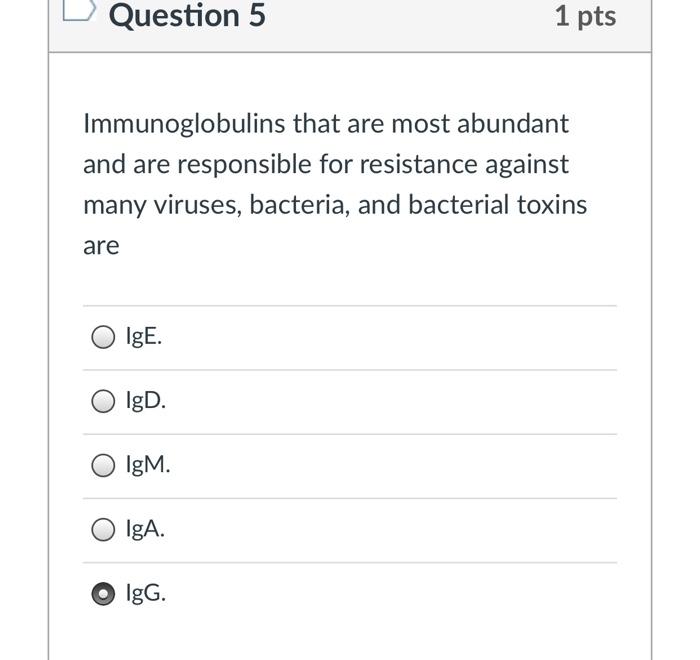
IgG is the most abundant antibody in human blood, constituting approximately 75-80% of all immunoglobulins. Its structure is exquisitely designed for versatility and is characterized by a Y-shaped form, which provides numerous binding sites for antigens, much like a multi-faceted key can unlock various doors. This configuration allows IgG to engage effectively with a wide array of pathogens, including bacteria and viruses, thereby neutralizing potential threats before they can cause harm.
The transition of IgG from maternal circulation to fetal immunity begins around the second trimester of pregnancy. As the fetus grows and develops, the maternal immune system begins to produce specific IgG antibodies in response to pathogens that may threaten both mother and child. These antibodies are then transported through the placenta, where specialized receptors facilitate the passage, ensuring the fetus is equipped with an arsenal of immune defenses by the time of birth. This transfer is not a random act but a carefully orchestrated exchange, ensuring that the newborn receives immunity to diseases to which the mother has been exposed.
A mother’s IgG also plays a pivotal role in passive immunity. Unlike active immunity, which develops when the immune system responds to pathogens through vaccination or infection, passive immunity occurs when antibodies are transferred from one individual to another. In the delicate scenario of pregnancy, this transfer is truly life-saving. As the infant enters a world teeming with pathogens, maternal IgG provides a shield against infections during the early months of life, a critical period when the infant’s immune system is still maturing.
Despite the protective nature of maternal IgG, it is paramount to recognize the importance of timing and specificity. The antibodies transferred provide immunity against the diseases to which the mother has been previously exposed. For instance, if a mother has been vaccinated against tetanus or measles, her IgG will convey protection to her child against these diseases. However, if the mother has not encountered certain pathogens or has not been immunized, the infant may remain vulnerable. This underscores the essential need for maternal immunization during pregnancy, enabling the mother’s immune system to generate specific IgG responses that can be shared with the fetus.
The remarkable journey of IgG illustrates the intricate interdependencies of life. It is a powerful testament to the protective mechanisms that have evolved over millennia, ensuring that infants can survive their initial foray into a world filled with microbial challenges. However, this journey does not end at birth; while maternal IgG provides a strong initial defense, it gradually wanes over the first year of life, prompting the need for active immunization through vaccines. This cycle of passive to active immunity epitomizes the vital continuity of protection from mother to child, fostering resilience against infectious diseases.
This delicate interplay extends beyond the realms of biology; it provides a profound metaphor for nurturing and protection. The transfer of IgG signifies more than just immunity; it embodies the deep connection between mothers and their offspring, encapsulating love, sacrifice, and an enduring commitment to safeguarding the future. In essence, the immune system is a reflection of the life-giving bond between mother and child, where the act of transferring antibodies is akin to passing down a legacy of strength and resilience.
In summary, the ability of IgG antibodies to traverse the placenta exemplifies the marvels of human physiology and maternal-fetal relationships. While it serves a critical role in imparting immunity, it also invites broader reflections on the nature of protection in the human experience. As we continue to explore the complexities of immunology and maternal health, we uncover not only the biological intricacies at play but also the profound stories woven within the fabric of life. Understanding this intricate relationship between antibodies and maternal immunity reassures us of nature’s design—a protective embrace that origins long before a child takes its first breath.
