In the intricate and often tumultuous river of the human circulatory system, thrombi, or blood clots, can act as formidable putrid obstructions. They are like boulders strewn in a once-majestic stream, altering the course of a life-giving flow. When a thrombus forms, it can lead to dire consequences such as strokes, heart attacks, or pulmonary embolisms. In the world of pharmacology, there exists a specialized class of medication known as thrombolytics. These agents—often likened to the diligent work of nature’s own raindrops eroding massive rocks—dissolve thrombi and restore the flow of life. This article delves deeply into the pharmacodynamics, mechanisms of action, and clinical implications of thrombolytic agents, providing a comprehensive understanding of their role in modern medicine.
The Essence of Thrombolytics
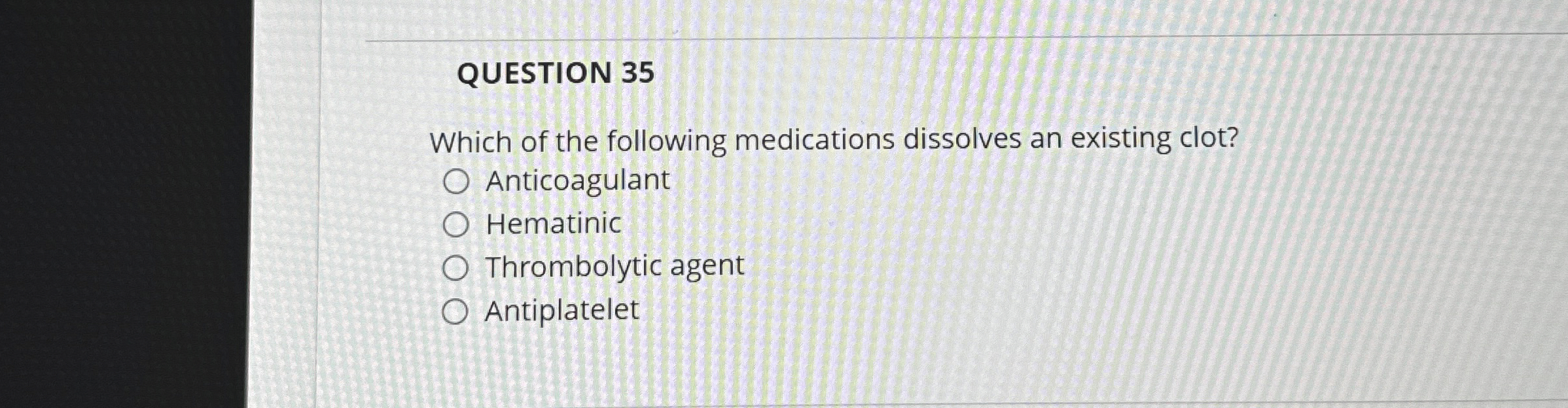
Thrombolytic agents, also referred to as “clot busters,” are pharmacological compounds that facilitate the breakdown of fibrin, a key protein in blood clot formation. By targeting the very core of thrombi, these medications usher in a transformative process, akin to the dismantling of barriers in a natural environment. Instead of simply compressing the boulder-like thrombus into smaller fragments, thrombolytics meticulously dissolve these obstructions entirely, restoring unobstructed circulation.
The Mechanism of Action
At the heart of thrombolysis lies the conversion of plasminogen into plasmin, an enzyme with the remarkable ability to degrade fibrin networks. Thrombolytic agents can be classified into two categories based on their sources and mechanisms: fibrin-specific and non-fibrin specific agents. The former, such as alteplase, resemble voracious predators selectively hunting down their prey within the fibrin matrix. In contrast, non-specific agents like streptokinase act more broadly, akin to the sweeping actions of a storm that removes debris from any surface it encounters.
The conversion process is initiated when thrombolytics bind to fibrin in the thrombus, promoting the activation of plasminogen. This is where the magic happens—plasminogen, upon activation, unleashes plasmin, which then exquisitely dismantles the fibrin structure. This enzymatic cascade mirrors the gradual yet relentless dissolution of a once-impassable dam, allowing the blood to flow freely once again.
Clinical Applications of Thrombolytics
Thrombolytics hold a pivotal role in acute medical scenarios, such as ST-Elevation Myocardial Infarction (STEMI), where swift intervention is crucial. The ‘golden hour’ in medical emergencies could very well be defined by the initial minutes post-chest pain, as time is of the essence. Administering thrombolytics can significantly decrease morbidity and mortality rates associated with cardiac events. Their utilization extends beyond the cardiac realm; treating acute ischemic strokes also benefits from the timely administration of these medications. By re-establishing perfusion to cerebral tissues, thrombolytics can mitigate long-term neurological sequelae.
Additionally, these agents are leveraged in cases of massive pulmonary embolism, often serving as a lifeline to patients grappling with life-threatening occlusions.
Challenges and Considerations
While the therapeutic potential of thrombolytics is substantial, they are not devoid of risks. The specter of hemorrhagic complications looms large, given that the dissolution of clots can inadvertently interfere with hemostasis elsewhere in the vascular system. Medical professionals must weigh the benefits against potential pitfalls judiciously, employing stringent selection criteria for candidates. A thorough understanding of contraindications—such as previous intracranial hemorrhage or severe uncontrolled hypertension—is essential in the decision-making process.
Furthermore, individual variation in response to these medications, influenced by factors like genetic polymorphisms or existing comorbidities, necessitates personalized therapeutic approaches. In some cases, the ripple effects of administering thrombolytics can propagate various outcomes, making clinician vigilance imperative.
The Future of Thrombolytic Therapy
Advancements in technology and pharmacology herald a new dawn for thrombolytic therapies. Research is actively exploring the development of more targeted agents that enhance efficacy while reducing risks. The potential amalgamation of thrombolytics with novel adjuvants, such as antiplatelet agents or anticoagulants, may result in synergistic effects that transform therapeutic paradigms. Furthermore, ongoing studies into microscale delivery systems—akin to surgical precision strikes—aim to optimize drug delivery to specific targets within the body, potentially revolutionizing treatment efficacy.
Conclusion
The world of thrombolytics is a testament to the delicate balance within our intricate biological ecosystems. Just as natural forces sculpt landscapes through gradual dissolution, thrombolytic medications navigate the complexities of human physiology, remolding pathways for blood flow. By demolishing thrombi, they enact a powerful pharmacological response that has the potential to save lives and herald recovery. As science progresses, the promise of a future where thrombolytics are even more refined, safer, and efficacious looms on the horizon, leading us toward a more enlightened era of medicine and patient care.
